treatments
Possible treatments depending on the pathologies
Treatments by pathology
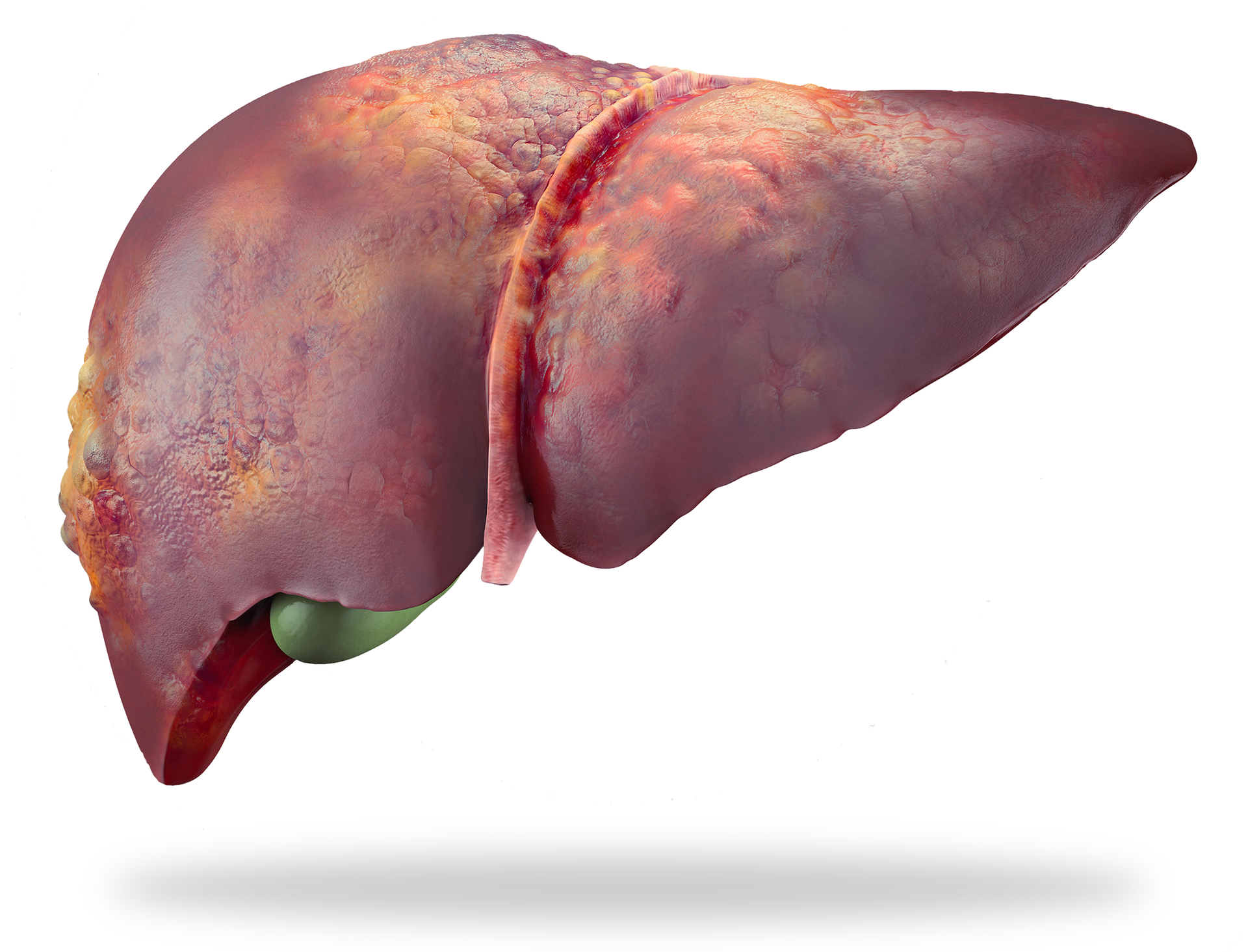
Liver surgery has evolved significantly in recent years thanks to advances in minimally invasive technologies. These techniques, such as laparoscopy and robotic surgery, offer many advantages over traditional methods. Laparoscopy, also known as laparoscopic surgery, allows for procedures to be performed with small incisions, reducing postoperative pain, speeding up recovery, and reducing the risk of infection. The surgeon uses a camera and specialized instruments to access the liver, providing a precise, real-time view of the area to be operated on. Robot-assisted surgery, on the other hand, is an even more sophisticated advancement. Using a robot, the surgeon can perform extremely precise movements thanks to miniaturized instruments and high-definition 3D visualization. This technology allows for more precise intervention, particularly for hard-to-reach tumors or delicate areas of the liver. Benefits include a shorter hospital stay, faster recovery, and smaller scars, which also improve the cosmetic outcome. These innovations allow patients to benefit from safer and less invasive treatment. However, the decision to use these techniques always depends on each individual case and the surgeon's expertise. Technological advances open new perspectives for the treatment of liver diseases, thus improving the quality of life of patients after surgery.
-
Patients
Surgical treatment is generally reserved for single or multiple tumors located in the same liver segment and for patients with preserved liver function without clinically significant portal hypertension. The treatment and personalized care plan (PCP) will be outlined to the patient during a dedicated pre-surgery consultation. Patient selection for surgery depends on several factors such as underlying liver function, remaining liver volume, and the presence or absence of portal hypertension. Patients must undergo a series of preoperative tests to assess their health status and suitability for surgery based on these criteria.
-
Objective
The primary goal of surgical treatment is to completely remove the cancerous tumor while preserving remaining liver function. New techniques, including laparoscopy, allow for less invasive surgery, with faster recovery and fewer postoperative complications. Laparoscopy is a minimally invasive surgical technique that uses thin instruments and a small tube equipped with a camera to view the inside of the body. This technique allows for more precise and less invasive surgery for patients with hepatocellular carcinoma.
-
Effects & Monitoring
Side effects of surgery may include postoperative pain, fatigue, loss of appetite, nausea and vomiting, and decompensation of cirrhosis. Post-treatment monitoring is important to detect any recurrence or recurrence of the tumor. Patients will be followed regularly by their primary care physician, and imaging tests, such as CT scans or MRIs, will be performed every 3 months to monitor the progression of the disease.
-
Conclusions
In conclusion, surgery is an effective treatment option for patients with hepatocellular carcinoma presenting with one or more lesions located in the same segment of the liver but reserved for patients with preserved liver function and in the absence of significant portal hypertension. New techniques such as laparoscopy allow for less invasive surgery with faster recovery and fewer postoperative complications.
IN SURGERY
For HCC or cholangiocarcinoma cancer
Percutaneous ablation
For HCC or cholangiocarcinoma cancer
Microwave ablation (MW) is a thermal ablation procedure that uses electromagnetic waves to destroy liver tumors with heat. Cryotherapy destroys lesions with cold, and electroporation, a newer technique, uses high-intensity electrical currents for the same purpose. The choice between these different techniques is made depending on the location of the tumor in the liver.
These techniques are often used to treat small liver tumors (< 3 cm) or when surgery is not an option.
-
Goals
Surgical treatment is generally reserved for single or multiple tumors located in the same liver segment and for patients with preserved liver function without clinically significant portal hypertension. The treatment and personalized care plan (PCP) will be outlined to the patient during a dedicated pre-surgery consultation. Patient selection for surgery depends on several factors such as underlying liver function, remaining liver volume, and the presence or absence of portal hypertension. Patients must undergo a series of preoperative tests to assess their health status and suitability for surgery based on these criteria.
-
Terms and Conditions
- The treatment method depends on the stage of the disease and the size of the tumor. External beam radiotherapy is usually administered in several sessions over a period of several weeks. During each session, patients lie on a treatment table and a radiotherapy machine is used to deliver a precise dose of radiation to the tumor. Anesthesia is not required. Note that this technique is not indicated for patients with:
- Unpreserved liver function
- Extrahepatic metastases
- Certain blood test abnormalities.
External radiotherapy
For HCC or cholangiocarcinoma cancer
Liver tumors such as hepatocellular carcinoma and cholangiocarcinoma can benefit from external radiotherapy treatment. The choice of this treatment will be made during a multidisciplinary consultation meeting (RCP) bringing together all the specialists involved in the management of liver tumors (surgeons, hepatologists, oncologists, radiologists, radiotherapist, etc.) and will depend on the size and location of the tumor, the presence or absence of metastases, but also the function of the healthy liver. External radiotherapy treatment is generally reserved for single tumors, not amenable to treatment by surgery or ablation or intraarterial (chemoembolization, radioembolization) and for patients with preserved liver function. The treatment and the personalized care plan (PPS) will be presented to the patient during the RCP during a dedicated announcement consultation.
-
Goals
Radioembolization treatment is generally reserved for single tumors, not amenable to treatment by surgery, ablation, or chemoembolization, and for patients with preserved liver function. This treatment may also appear as a waiting treatment before surgery or liver transplantation. The treatment and personalized care plan (PCP) will be presented to the patient during a dedicated consultation during the MTR.
-
Technique
Radioembolization is an interventional radiology technique performed by a radiologist that takes place in two stages: The first stage is the preparatory phase. In interventional radioligy, a catheter is introduced into the femoral artery, located at the root of the thigh, or through the radial artery located at the wrist, and then directed towards the hepatic artery. Once the catheter is positioned near the tumor, the radiologist checks the tumor vascularization and injects the preparation based on micro-aggregates of radioactive albumin into the tumor. The product, non-toxic, makes it possible to verify the good fixation of the product at the tumor level and the absence of fixation outside the tumor at the liver level and the absence of fixation elsewhere in the body. The patient is then transferred to nuclear medicine to undergo a scintigraphy. This examination is painless. The second stage is the therapeutic phase which will take place in a similar way to the preparatory phase unlike the injection of radioactive beads. This intervention is performed under local anesthesia.
-
Effects & Monitoring
Radioembolization can be performed as a short-term inpatient procedure, usually for 2-3 days per treatment phase, or as an outpatient procedure depending on the center. The procedure may be associated with side effects such as nausea, fatigue, and mild abdominal pain. These side effects are usually temporary and can be managed with medication or symptomatic treatments. Post-treatment monitoring helps assess treatment response. Patients will be followed regularly by their primary care physician, and imaging tests, such as CT scans or MRIs, will be performed every 3 months to monitor disease progression. The true effectiveness of the treatment is generally assessed approximately 6 months after treatment due to the prolonged action of the radiation.
-
Conclusions
In conclusion, radioembolization is an effective treatment option for patients with hepatocellular carcinoma not amenable to surgery, ablation, or chemoembolization, which allows direct targeting of cancer cells in the liver with minimal side effects. Note that this technique is not indicated in patients with: - Unpreserved liver function; - Renal failure; - Extrahepatic metastases; - Major heart failure; - Certain blood test abnormalities.
radio embolization
For CHC cancer
Liver tumors such as hepatocellular carcinoma and cholangiocarcinoma can benefit from treatment by radioembolization, also known as selective internal radiotherapy. The choice of this treatment will be made during a multidisciplinary consultation meeting (RCP) bringing together all the specialists involved in the management of liver tumors (surgeons, hepatologists, oncologists, radiologists, radiotherapist, etc.) and will depend on the size and location of the tumor, the presence or absence of metastases, but also the function of the healthy liver.
-
Goals
Chemoembolization treatment is generally reserved for multiple tumors, not amenable to surgical or ablation treatment, and for patients with preserved liver function. This treatment may also appear as a waiting treatment before surgery or liver transplantation. The treatment and personalized care plan (PCP) will be presented to the patient during a dedicated consultation during the multidisciplinary meeting.
-
Technique
- Chemoembolization is an interventional radiology technique performed by a radiologist that involves two steps:
- A fatty substance is injected into the arteries near the tumor, mixed with a chemotherapy product designed to destroy liver tumor cells through a cytotoxic effect.
- Blood circulation within the tumor vessels is significantly reduced, or even eliminated, using embolization agents. This technique thus makes it possible to act specifically on tumors while preserving healthy liver tissue. There is no need for general anesthesia for this type of intervention and chemoembolization treatment is carried out in a short hospitalization, generally for 2-3 days. The procedure begins with a puncture of the radial or femoral artery, followed by catheterization to access the hepatic artery and inject the mixture of chemicals and particles into the tumor. Depending on the number of lesions and their location, several successive procedures spaced 4-6 weeks apart may be necessary to control the disease.
chemo embolization
For CHC cancer
Patients with hepatocellular carcinoma or neuroendocrine tumors may benefit from chemoembolization treatment. The choice of this treatment will be made during a multidisciplinary consultation meeting (RCP) bringing together all the specialists involved in the management of liver tumors (surgeons, hepatologists, oncologists, radiologists, radiotherapist, etc.) and will depend on the size and location of the tumor, the presence or absence of metastases, but also the function of the healthy liver.
Patient pathways
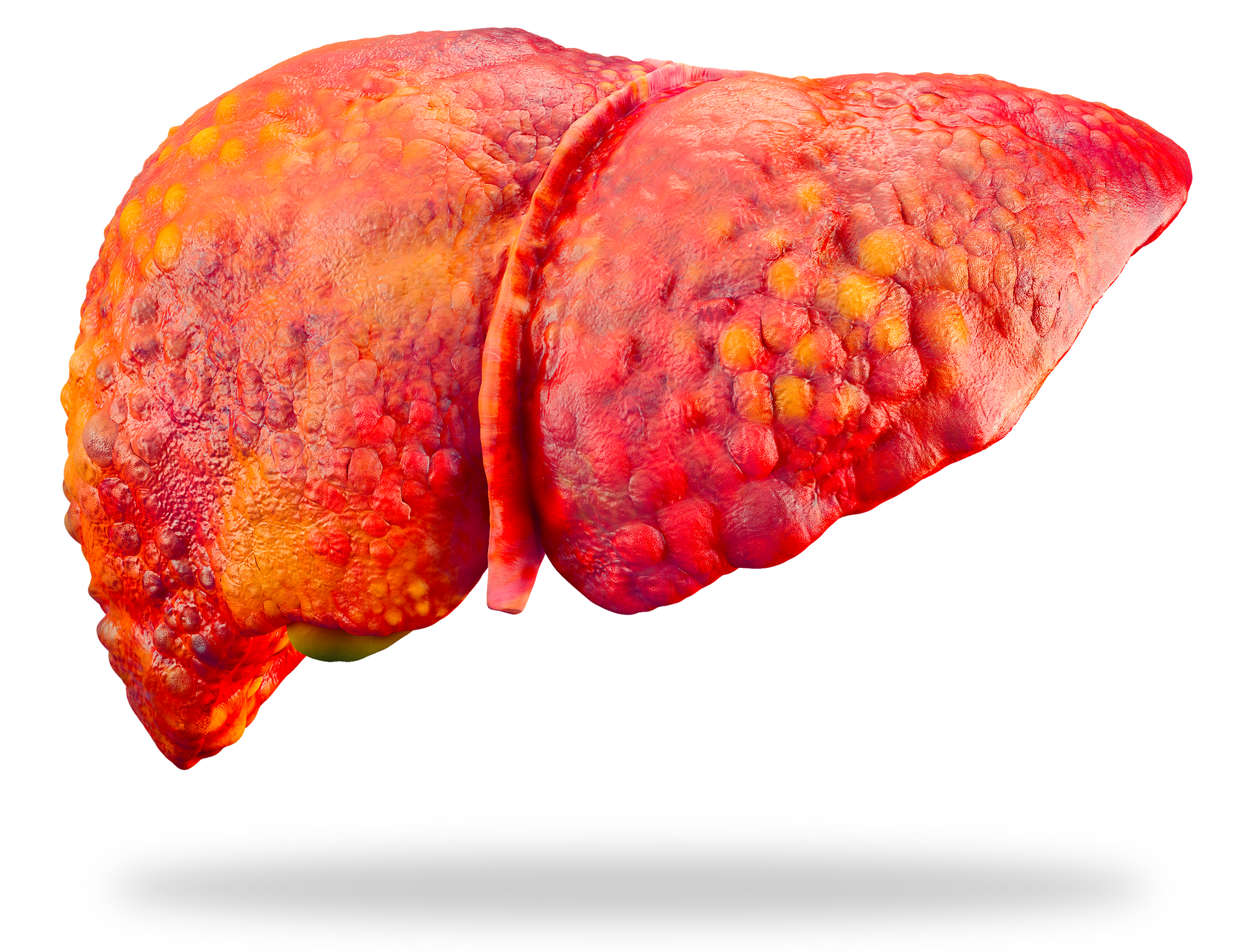
for patients with liver cirrhosis
When it comes to liver disease and its treatment, the patient pathway is of great importance. It will allow you, as a patient, to personalize your care pathway, from assessment to RCP, from hospitalization to consultations with internal or external specialists, the patient pathway allows you to better manage all phases of the disease.